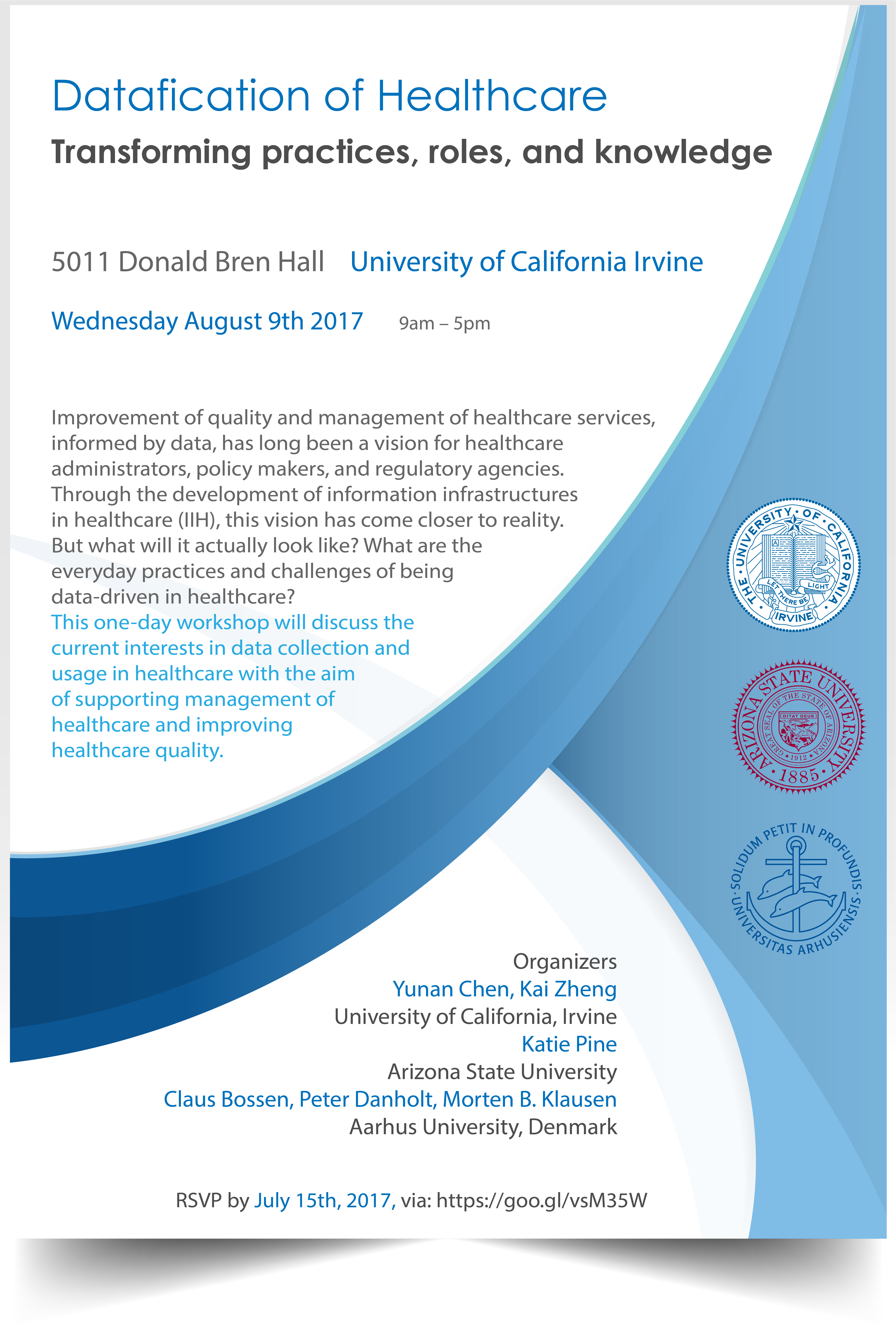
Workshop on “Datafication of healthcare: Transforming practices, roles, and knowledge”
Wednesday August 9th 2017 9am – 5pm
Location: 5011 Donald Bren Hall, University of California Irvine
Please RSVP by July 15, 2017 via this link.
Organizers:
Yunan Chen, University of California, Irvine Kai Zheng, University of California, Irvine Katie Pine, Arizona State University Claus Bossen, Aarhus University, Denmark Peter Danholt, Aarhus University, Denmark Morten B. Klausen, Aarhus University, Denmark
Background:
This one-day workshop will discuss the current interests in data collection and usage in healthcare with the aim of supporting management of healthcare and improving healthcare quality.
Improvement of quality and management of healthcare services, informed by data, has long been a vision for healthcare administrators, policy makers, and regulatory agencies. Through the development of information infrastructures in healthcare (IIH), this vision has come closer to reality. But what will it actually look like? What are the everyday practices and challenges of being data-driven in healthcare?
IIHs have made available an unprecedented amount of data to monitor healthcare quality and output as well as reconfiguring the structures of governance, placing policy and protocols into the technical core of organizational functioning. One early example from the 1990s is the reporting of data concerning Diagnosis-Related Groups (DRG) as a way to link budgets, payments, and clinical activities. Presently, the implementation of electronic health records (EHR) has made data about healthcare services more easily available and accessible for researchers, organizational stakeholders, and governmental agencies. Recently, through ‘patient reported outcome measures’ (PROM), data upon laypersons’ health, after or during prolonged treatments out of medical settings, are collected and constantly monitored. Over the years, a number of governance strategies for healthcare such as ‘triple aim’ (Brewster), ‘capitation’ (James & Poulsen), ‘value-based healthcare’ (Porter & Teisberg), and `accountable healthcare organizations’ (Fisher et al.) have been suggested to simultaneously curb rising healthcare costs and improve quality of care in the U.S. and other industrialized countries. Common to all of these strategies is the need to generate data about healthcare services. The quantification of healthcare performance in certain data-driven metrics makes performance seeable and “manageable,” allowing implementation of these new governance strategies at organizational, regional, and national levels.
However, generation of data and construction of infrastructures for accountability and quality improvement of healthcare organizations require bringing together multiple stakeholders as well as attending to the technical aspects of creating, accumulating, curating, and presenting data. Also, acting upon data is not always straight forward, and involves transforming data to information and subsequently knowledge and actions. Unintended consequences are inevitable and must be examined as well.
Aims and purpose of the workshop:
Through this workshop, we are interested in exploring similarities and differences in datafication initiatives and exploring their relations to specific sites, and local contexts and practices as both an attempt at doing infrastructural inversion (Bowker & Star, 1999), i.e. learning to see what is otherwise hidden, as well as insisting on the situatedness and locatable quality of data and datafication in opposition to ideas about data as universal and detached. We are also interested in how datafication of healthcare transforms the roles of different actors such as clinicians, clerical staff, patients, care givers, healthcare administrators and decision-makers. We believe that a better understanding of these issues is crucial for both understanding the effects of datafication and for building purposeful healthcare data infrastructures, and properly using the vast amount of data produced to monitor and improve the quality and management of healthcare. Since the workshop organizers are based in both the U.S. and out of Scandinavia comparisons and establishing ‘partial connections’ (Strathern 2004), the intention of the workshop is to stimulate learning, thinking and discussion by bringing the organizers' specific knowledge of their contexts into conversation and comparison with respect to the datafication of healthcare.
Lastly, the workshop is intended to explore the possibilities for future collaboration between the participants. In this workshop, we will discuss:
- Are current healthcare information infrastructures optimized for supporting clinical work, or for revenue management? How can these dual functions be supported? - What types of new competences, skills, and roles are required to improve the recording, use, and reuse of healthcare data in the health IT era? - How to achieve the value of healthcare data for quality and management improvement purposes? - What are the central issues for designing and using health IT to achieve the goal of data-driven quality improvement and management in healthcare? - What are potential unintended consequences of the emerging regime of data-driven management and quality improvement for healthcare workers and healthcare organizations? How can these unintended consequences be mitigated? - How to ethnographically research, follow and analyse datafication and information infrastructures and their consequences given their multisited, virtual and abstract qualities.
Workshop format and schedule:
The one-day workshop welcomes all researchers, practitioners, and students who are interested in the above issues to participate. Participants are encouraged, but not required, to submit an abstract (max 300 words) in which they briefly outline their research interest and questions in relation to datafication of healthcare. Participant with abstracts will have 10 min. for presentation at the workshop of their work and interests.